What is glaucoma?
Glaucoma is a disease that causes damage to the optic nerve. The optic nerve, which acts as a messenger for information between the eye and the brain, is in the back of the eye. When the nerve is damaged, a loss of vision is likely to occur. Initially, people with glaucoma will lose their peripheral (side) vision. If the disease remains untreated, vision loss will likely get worse. This can lead to total blindness over time.
Laser Eye Surgery of Erie
The two basic glaucoma types
Glaucoma often presents with no symptoms to warn you. Detecting and treating the disease early is important to prevent blindness. Treatments are available and early detection is critical.
Open-Angle Glaucoma
Open-angle glaucoma is the most common form of the disease. The risk of developing open-angle glaucoma increases with age. It has no symptoms in its early stages and vision is normal. As the optic nerve becomes more damaged, blank spots begin to appear in your field of vision. Patients can experience:
- Gradual loss of side or peripheral vision
- An inability to adjust the eye to darkened rooms
- Rainbow-colored rings or halos around lights
Closed-Angle Glaucoma
Closed-angle glaucoma (also called angle-closure glaucoma) is more rapid symptoms. Patients may experience:
- Blurred vision
- Severe eye pain
- Rainbow-colored halos around lights
Narrow-angle glaucoma can precede closed-angle glaucoma. Treatment for both closed-angle and narrow-angle glaucoma include a laser peripheral iridotomy or a iridectomy. The treatment creates an alternate route for the fluid in the eye flow and prevents pupillary block so the eye pressure does not increase. Risk factors for closed-angle glaucoma include:
- Hyperopia (far-sightedness)
- Cataracts
- Over the age of 55
Research has shown that cataract surgery can treat and reduced the risk of narrow-angle and closed-angle glaucoma.
Glaucoma Risk Factors
Regular medical eye exams can help prevent unnecessary vision loss. People who are at a greater risk for glaucoma usually have the following conditions:
- Age: You’re at higher risk if you’re older than 40.
- Ethnic Background: Certain ethnicities, such as African-Americans, are at risk of developing the disease at a younger age and are more likely to experience permanent blindness as a result.
- Family History: Glaucoma may have a genetic link; therefore, if you have a family history, you are at a greater risk of developing the condition.
- Medical Conditions: Diabetes, heart disease, high blood pressure and hypothyroidism are several conditions that may increase the risk of developing this disease.
- Other Eye Conditions: Eye tumors, eye inflammation, lens dislocation and retinal detachment could increase the risk of glaucoma. Certain types of eye surgery and being nearsighted or farsighted may also increase your risk.
- Injury: Increased eye pressure is sometimes a result of severe eye injuries; therefore, trauma can increase the risk of developing this disease.
- Long-term Corticosteroid Use: Corticosteroid medications (e.g. some eye drops) over a long period of time may increase the risk of developing glaucoma.
Early Detection is Key
Comprehensive eye exams are necessary to diagnose glaucoma. We will measure your eye pressure, dilate your pupils to evaluate your optic nerve and perform a visual field test to measure your peripheral vision. Initially, eye drops are usually used treat glaucoma, but sometimes laser would be considered first. Resistant and severe glaucoma may need surgery. See the “glaucoma surgery” link for more information.
Glaucoma Laser
A selective laser trabeculoplasty (SLT) and argon laser trabeculoplasty (ALT) are both very similar laser procedures to reduce the eye’s pressure. This is done in the office by placing a special contact lens on the eye. The laser is then focused through this lens to the angle of eye (trabecular meshwork). The laser helps improve aqueous outflow which in turn helps reduce the eye’s pressure.
Goniotomy
A Goniotomy is a Minimally Invasive Glaucoma Surgery (MIGS) which can lower intraocular pressure by improving the outflow dynamics of the eye. It was originally used to treat Glaucoma in children, but has been adapted to treat mild to severe Glaucoma in adults.
A Goniotomy opens the eye’s natural fluid drainage pathway by removing part of the trabecular meshwork. By opening the eye’s natural fluid drainage pathway, the intraocular eye pressure should decrease. There is no need for a stenting device with this procedure. A Goniotomy can be performed with or without Cataract Surgery. The post-operative care and follow-up is similar to Cataract Surgery.
The most common instrument to perform a Goniotomy is a KDB Glide. Below is a diagram demonstrating the removal of the trabecular meshwork.
Treating Your Glaucoma
The iStent® is yet another way to treat mild to moderated glaucoma. The FDA requires this procedure to be performed in conjunction with cataract surgery. If you have already had cataract surgery you are not a candidate for this procedure.
If you have glaucoma, over time your eye’s natural drainage system becomes clogged. iStent® creates a permanent opening through the blockage to improve the eye’s natural fluid outflow. By improving the outflow of fluid in your eye, iStent® is designed to lower and control the pressure within your eye.
The iStent® Trabecular Micro-Bypass Stent is 20,000 times smaller than the intraocular lens (IOL) your doctor will use to replace your cataracts. By increasing your eye’s ability to drain fluid, this technology is designed to improve the aqueous outflow to safely lower your eye pressure.
If you are a candidate for the iStent® then your surgeon can implant it during your cataract surgery procedure. Once implanted, the iStent® will begin working to safely and effectively manage your eye pressure.
See below step-by-step Trabeculectomy.
The basic goal behind trabeculectomy is to create a small hole in the anterior chamber of the eye to allow drainage of the aqueous fluid toward the outside. Trabeculectomy surgery starts with making an incision through the conjunctiva. Underneath the scleral flap, a surgeon cuts a small hole into the anterior chamber, which allows the drainage of aqueous fluid through the scleral flap and into the sub-conjunctival space. An iridectomy (hole in the iris) is performed at this point to allow the scleral opening to stay open without being blocked by the iris tissue. The scleral flap is then tied down with stitches, that are loose enough to allow continuous drainage of the aqueous fluid. Finally, the overlying conjunctival tissue is closed with stitches to allow formation of a bleb or an elevation of conjunctival tissue formed by the aqueous fluid, which is being filtered out of the scleral flap (trapdoor) underneath. The filtering bleb is usually located in the superior aspect of the eye and covered by the upper lid. It is not readily noticeable by a casual observer. The aqueous fluid from the filtering bleb is then slowly absorbed by the conjunctival and episcleral (on the surface of the sclera) blood vessels and drain into the orbital venous system.
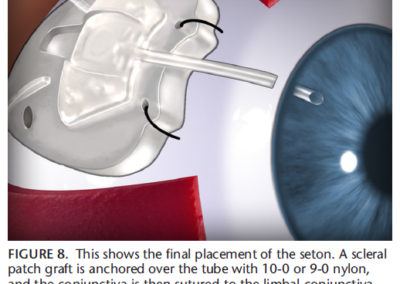
Seton Implant
The basic goal of a seton implant is to decrease the eye’s pressure. A tube is inserted into the anterior chamber so the aqueous fluid can drain into the seton implant and out of the anterior chamber of the eye. The implant is sutured into a conjunctival pocket and the aqueous is absorbed naturally.
The diagram below shows the step-by-step insertion of a Ahmed Valve ® which is one of the most common seton implant.
Laser Eye Surgery of Erie
Additional Services
PTK and Amniotic Tissue Graft
Home Phototherapeutic Keratectomy (PTK) Phototherapeutic Keratectomy (PTK) and Amniotic Membranes with bandage contacts play an important role in treating…
read more
Corneal Transplants
Corneal transplants are required for a number of corneal diseases and a variety of other reasons. Before and after transplant,…
read more
Dry Eye
Dry eye occurs when people don’t produce enough tears or the right quality of tears to keep their eyes healthy…
read more
Diabetic Services
Diabetic retinopathy is a disease that affects diabetic people and eventually leads to blurry, distorted vision and blindness. When people…
read more
Macular Degeneration
Age-related macular degeneration (AMD) is a deterioration or breakdown of the eye’s macula. The macula is a small area in…
read more
Glaucoma Surgery and MIGS
iStent works like the stents used to prevent heart attacks and strokes. When blood vessels get clogged, a stent creates…
read more
Retinal Surgery
The retina is a thin sheet of nerve tissue in the back of the eye where light rays are focused…
read more
Keratoconus & Corneal Cross Linking
Keratoconus, often referred to as ‘KCN’, is a non-inflammatory eye condition in which the typically round dome-shaped cornea progressively thins…
read more
Glaucoma
Although glaucoma is the leading cause of blindness in Americans, early detection can prevent you from losing your eyesight. In…